Buy One, Get One 50% OFF Eyeglasses
* Restrictions apply. Ask a Team Member for details.
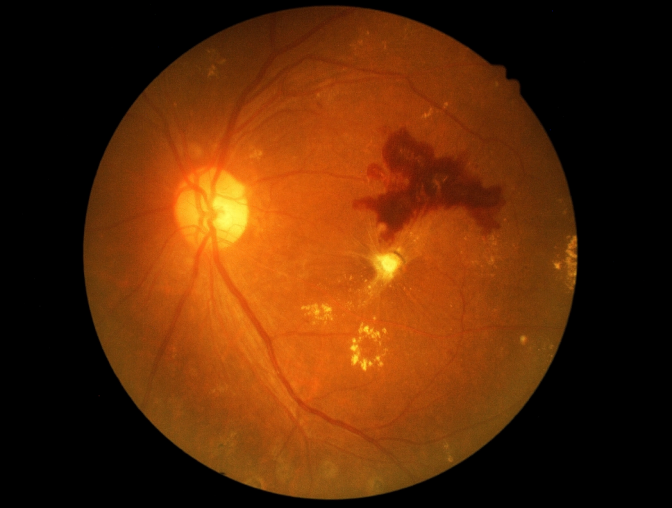
What is Diabetic Retinopathy?
Diabetics are at risk for developing diabetic retinopathy, a condition that damages the retina within the eye. The longer you live with diabetes, the more likely it is that you will experience this complication. A healthy retina is important for maintaining good vision. The retina is the light-sensitive structure on the inner back wall of the eye. When light enters your eye, an image of what's in your field of vision appears on the retina. The retina transmits these light signals through the optic nerve to the brain, which then translates the signals into images your brain can understand.
A network of tiny blood vessels keeps the retina healthy and functioning. People with diabetes that have high blood pressure or uncontrolled blood sugar levels may experience damage to the small blood vessels throughout the body, including the vessels in the eye. The retina may not receive enough blood flow to maintain proper function or the damaged blood vessels may leak small amounts of blood into the eye, leading to vision loss. In some cases, abnormal blood vessels may form within the retina, which may lead to worsening fluid leakage or the formation of scar tissue, both of which may contribute to vision loss.
What Are Symptoms of Diabetic Retinopathy?
At first, people who develop diabetic retinopathy may not notice any vision changes because the symptoms are silent in the condition's early stages. When diabetic retinopathy becomes more advanced, it may affect vision in a number of ways:
Your vision may appear blurry
You may notice floaters in your field of vision
Your night vision may worsen, or you may begin to see colors less vividly
You may see dark spots or unexpected blank areas within your field of vision
If you have diabetes and notice any of these vision problems, call your eye doctor for an appointment to assess your eye health.

How Do Eye Doctors Diagnose Diabetic Retinopathy?
An eye doctor can assess your retinal health during a comprehensive eye exam. The doctor will dilate your pupils with eye drops to better examine the inner structures of your eyes.
The doctor may perform a test known as optical coherence tomography, which takes images of the retina to assess its thickness to check for the presence of diabetic retinopathy.
A fluorescein angiography may also be administered. This testing method helps the eye doctor view the blood vessels in your retina. The doctor will begin by injecting dye into your arm, which travels through blood vessels and reaches your eyes. The dye appears bright yellow, making it easy to see the tiny blood vessels that may be damaged by diabetic retinopathy. Using a specialized camera, the doctor takes images of your eyes to see if the blood vessel activity indicates an eye condition related to diabetes.

How Do Doctors Treat Diabetic Retinopathy?
In early stages of the diabetic retinopathy, managing your diabetes may be enough to keep the eye condition under control. It is important for people with diabetes to visit an eye doctor regularly for a dilated eye exam to keep track of any structural changes to the eyes.
When diabetic retinopathy develops into more advanced stages and begins to affect your ability to see, treatment may help to preserve your remaining vision. A medication known as anti-VEGF therapy can stop blood vessels from leaking inside the eye and is injected into the eye after it is numbed. Laser treatments may also be used to seal leaky blood vessels and minimize the development of new, abnormal blood vessels. If scar tissue or fluid are present inside the eye, surgery may be recommended to remove it.

How Should People with Diabetes Care for Their Eyes?
After you have developed diabetes, it is critical that you take any medication prescribed by your doctor to help keep your blood sugar levels in a healthy range. Seeing an eye doctor at least once a year for a dilated eye exam will help you keep tabs on your eye health and will allow your eye doctor to catch signs of diabetic retinopathy and other eye conditions early.
Good nutrition and regular physical activity will help to keep your blood sugar levels in a healthy range. Eating a healthy diet and getting regular exercise can also lower your risk of developing diabetic retinopathy or help to prevent existing retinopathy from worsening.
Diabetic retinopathy may lead to vision loss or blindness, but these complications are usually preventable with the management of diabetes and the supervision of an eye doctor.
